What Is Twin-to-Twin Transfusion Syndrome?
Twin-to-twin transfusion syndrome (TTTS) is a rare pregnancy condition that connects the circulatory system of certain twins. Approximately 6,000 babies each year might be affected by TTTS, according to the National Organization of Rare Disorders. Although this condition is rare, understanding more about it informs many aspects of maternal and fetal health care.
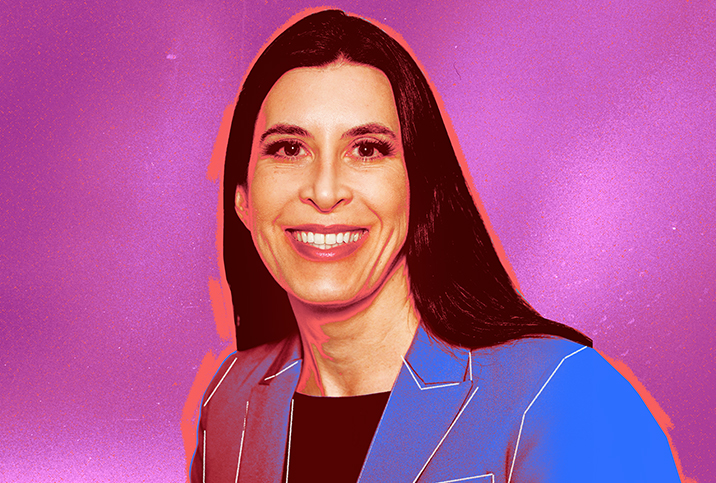
Genevieve Grabman, J.D., M.P.H., an attorney for United Nations agencies, author of "Challenging Pregnancy" and mother of four, experienced TTTS with her twins. While facing a complex and frightening pregnancy, Grabman also had to battle anti-abortion politics, which limited the care available to her and the doctors and hospitals willing to treat her. For more details on Grabman's experience, read Giddy's exclusive interview with her.
In this article, we talk about the TTTS condition itself. Alongside, Grabman discusses her physical experience with TTTS and touches on some of the politics involved in her care, which, ultimately, determined the outcome of her pregnancy.
What is TTTS?
TTTS is a rare condition that can sometimes occur in monochorionic twins, which are identical twins that share a placenta, according to Mert Ozan Bahtiyar, M.D., director of the Yale Medicine Fetal Care Center in New Haven, Connecticut, and an expert in diagnosing and treating complex abnormalities in babies before they are born.
Bahtiyar explained that, generally, the placenta in monochorionic twin pregnancies is divided into two portions, not necessarily physically but functionally, and each side of the placenta supports a different twin.
There are always blood vessel connections between each side, and the blood goes back and forth. Most of the time, each twin gets equal support. In about 10 percent to 15 percent of monochorionic twin pregnancies, however, one baby gets more blood than the other one. The "donor" twin gives too much blood to the "recipient" twin.
"It is an imbalanced blood transfusion between two babies that leads to TTTS," Bahtiyar said.
"One baby pumps away its blood to the other twin. So one twin [the donor] doesn't get enough nutrients, doesn't grow as well, becomes dehydrated, and doesn't urinate or produce enough amniotic fluid," Grabman explained. "Whereas the other twin [the recipient] is ballooning with fluid, passing lots of urine and creating a huge amount of amniotic fluid."
The donor twin is at risk of kidney and other organ failures because of inadequate blood flow. The recipient twin is at risk of heart failure and generalized soft tissue swelling (hydrops) because of the thick extra volume of blood.
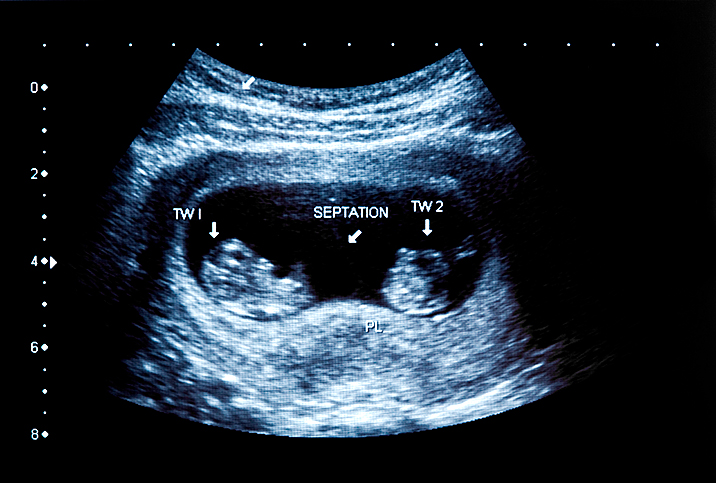
Diagnosing TTTS
"We don't know exactly how early TTTS can be recognized," Bahtiyar said. "However, usually, it is diagnosed at the 10- to 14-week ultrasound scan where nuchal screening takes place."
Nuchal translucency is a collection of fluid under the skin at the back of the baby's neck. Your healthcare provider measures the nuchal translucency to screen for conditions such as Down syndrome, also referred to as trisomy 21. It is also a predictive indicator for TTTS in a twin pregnancy.
An ultrasound scan can also show amniotic fluid levels, and TTTS is diagnosed by measuring these fluid levels. In TTTS, one twin has a high amniotic fluid level in the amniotic sac, while the other has a low level. Different sizes and weights of the twins are also telltale signs of the condition.
In Grabman's pregnancy, TTTS was recognized particularly early. She explained that the pregnancy didn't look viable on her ultrasound scan at first glance.
"It looked like a blighted ovum because the two embryos were so close together, couldn't be distinguished, and the amniotic sacs were not distinct," she said.
After thinking the pregnancy would not be viable, a doctor realized on a further ultrasound scan that, in fact, Grabman was carrying twins but the fetuses were not the size they should be for the stage of pregnancy. At this early stage of only eight weeks, the doctor suspected TTTS and referred Grabman to a specialist for further investigation to confirm the diagnosis.
Typically, most cases of TTTS are confirmed around 16 weeks of pregnancy, according to Bahtiyar.
What are the potential complications and risk factors of TTTS?
In TTTS, the babies are conjoined.
"They are not joined physically at the hip, head or any other part of the body, but they are conjoined at the placenta," Bahtiyar explained.
One of the most significant risks is the demise of one twin.
"If one baby dies during the pregnancy, the surviving baby can be affected and experience brain damage," Bahtiyar said. "Research shows that in 20 percent to 40 percent of the pregnancies where one twin dies, the surviving twin experiences brain damage."
"If one twin dies, it can pull down the health of the recipient twin, which, in some circumstances, can lead to early labor and delivery, and sometimes the death of both twins," Grabman said. "This is the biggest concern."
If TTTS is not treated, it can lead to preterm delivery.
"Both spontaneous and iatrogenic preterm birth is high in TTTS pregnancies," Bahtiyar stated.
An iatrogenic preterm birth is a planned delivery (initiated preterm birth) before 37 weeks of gestation. Preterm births are concerning, though common, in pregnancies of multiple fetuses because each fetus may be smaller and less developed than a singleton would be.
"Not all preterm births are equal. There is a big difference between a 24-week delivery, 28-week delivery and 34-week delivery. The goal is to support the mother to safely carry the pregnancy as long as possible to reduce the impact of preterm birth," Bahtiyar said.
What are the stages of twin-to-twin transfusion syndrome?
There are five stages of TTTS, as described by the Fetal Health Foundation:
- Stage I: The fetal bladder of the donor twin remains visible on ultrasound, but there is an imbalance in the amniotic fluid between the twins.
- Stage II: The donor twin's bladder does not fill with urine and is not visible on an ultrasound exam.
- Stage III: Excessive blood flow starts to cause problems with the recipient twin's circulation. Abnormalities in blood-flow patterns are identified via ultrasound.
- Stage IV: The recipient twin's heart begins to fail because of excessive fluid retention. Ultrasound identifies fluid collections around the abdomen and the chest.
- Stage V: One or both twins die from severe TTTS.
"It can stop progressing beyond stage I," Bahtiyar said. "We tell patients that, with stage I, a third get better, a third stay the same, and a third get worse. So we don't immediately recommend fetoscopic laser treatment."
For people who progress to stage II and beyond, the physician might recommend a specific type of fetal surgery, discussed in more detail below.
Historical treatment options for TTTS
In the past, Bahtiyar said doctors tried several treatment options for twin-to-twin transfusion syndrome.
"Delivery was one option," he said. "Another was prematurely rupturing the membrane between the twins to see if this balanced the pressure."
However, neither of these options worked.
"And, until quite recently, the option was to remove the excessive amniotic fluid. This was not therapeutic but aimed to extend the pregnancy further to reduce the risk of premature birth," Bahtiyar explained.
Grabman had her twins six years ago. In addition to the options laid out above—and monitoring the twins throughout the pregnancy—another treatment discussed at this time was umbilical cord occlusion, which results in selective termination of the donor twin, hopefully, leaving the recipient twin to survive.
Finally, fetal laser surgery had the best outcomes among the treatment options discussed with Grabman. At the time, this option was still relatively new.
"This was my preferred treatment option as it offered the best chance for both the twins and me to survive," Grabman stated. "The approval to have this surgery had to be made by a hospital ethics board. The three hospitals I consulted denied fetal laser surgery, despite my doctors advising this as the best course of action."
After denial of this treatment, the only option left for Grabman was monitoring.
"I was monitored closely to try and find the balance between fetal demise and preterm birth," Grabman said. "I knew I would have a preterm birth, but the goal was to try and move the needle so that the pregnancy continued as long as possible but not so long that a twin would die."
Current treatment options for TTTS
Bahtiyar said treatment options have progressed during the past 10 years. The aforementioned surgery, called laser fetoscopy (selective laser photocoagulation), has now become the gold standard treatment for TTTS.
Laser fetoscopy is a surgical procedure where a physician makes a small incision in the pregnant woman's abdomen. A tiny instrument equipped with a laser is inserted through the incision and used to burn the unequal blood vessel connections. A vacuum-assisted device then drains the excessive amniotic fluid from the area around the recipient twin.
"If a physician recognizes TTTS early, we can attempt to treat TTTS," Bahtiyar said.
The goal of the laser fetoscopy is twofold: to have two live babies and to try to prevent TTTS from getting worse.
"If there is no medical intervention, the odds of something extremely bad happening is extremely high," Bahtiyar added.
The surgery does come with risk: The biggest risk is rupturing the amniotic sac, leading to premature labor.
"There is no option without risk," Bahtiyar stated. "However, the surgery has less risk to the pregnancy than not treating TTTS at all.
"The research shows that for advanced-stage TTTS, if there is no intervention, there is a fetal fatality in more than 80 percent of cases for one or both twins," he added.
Side effects and symptoms of twin-to-twin transfusion syndrome
On the whole, the physical symptoms of a TTTS pregnancy are much the same as those of a normal pregnancy. In some cases, the mother-to-be may experience:
- The abdomen growing or expanding rapidly
- A sudden increase in body weight
- Increased abdominal pressure
- Shortness of breath
- Cramping or contractions
- Swelling of the hands and legs early in the pregnancy
"As the pregnancy progresses, the biggest difference is the pregnancy can look quite strange," Grabman said. "The abdomen can become very distended with amniotic fluid, even though one of the twins is starved of that fluid. So I looked quite weird at various stages of the pregnancy—not how I should have looked for that stage."
Bahtiyar stressed that it is important to look out for the following symptoms:
- Abdomen stretching too quickly
- Pelvic pressure
- Contractions
- Difficulty breathing
"These can be signs that fluid is accumulating very quickly and the body cannot adapt to it," he said.
"The most concerning symptom that I experienced was preterm labor and contractions from a very early stage, around 26 weeks gestation—it was frightening," Grabman said. "I was given medication to try and prevent labor [and] stop contractions, and steroid injections to speed up the development of the baby's lungs."
From 16 weeks on, Bahtiyar said the physician monitors the mother-to-be with an ultrasound every two weeks, and more frequently if there is any concern.
"There is no gold standard for how often to monitor; every country has slightly different guidelines," he said.
Managing TTTS requires specialized (and sometimes expensive) treatment
"In the U.S., you can't just show up at any hospital and give birth," Grabman said. "You need to attend a specialist center to ensure the best possible outcome for both the babies and yourself."
Only about 30 centers, perhaps a few more, offer laser fetoscopy in the United States, according to Bahtiyar.
"The distribution of these centers is not even across the country. However, most patients should be able to get access to a hospital that offers this procedure within a two-hour flight," he said.
A 2020 study published in the journal Fetal Diagnosis and Therapy investigated whether the distance traveled to a fetal treatment center is associated with adverse delivery and neonatal outcomes. This study found traveling a long distance to treat TTTS did not adversely affect pregnancy outcomes.
However, the study did not analyze the patients' socioeconomic status, and individuals with limited means may not be able to travel to access the gold standard surgery. And as Grabman experienced, some hospital ethics boards may not grant access to this treatment.
After Grabman gave birth, her twins needed to stay in the neonatal intensive care unit (NICU), one for three to four weeks and the other for six weeks. After being discharged home, they required a significant amount of care and medical intervention.
"The medical bills added up to over $1 million. I was very privileged that I had maternity leave, good medical insurance, and was able to access public assistance," Grabman said. "If policies dictate that every pregnancy is brought to term, there needs to be more assistance available and provision for the level of care these babies require."
A final note
"The most important thing I like to stress to all my patients with TTTS is that it is not due to something you have done or not done," Bahtiyar said. "This isn't something that you have caused. It is a random condition that you cannot predict or prevent."